Understanding Hypodermic Needle Gauges: The Key to Precise and Comfortable Medical Injections
When administering medications, vaccinations or drawing blood samples, healthcare professionals rely on hypodermic needles. These essential tools come in various sizes and gauges, and selecting the right one is crucial not only for accurate dosing but also for minimizing patient discomfort.
Understanding the nuances of hypodermic needle sizes plays a pivotal role in providing effective care. In this article, we’ll delve into the world of hypodermic needles and explore the factors that determine which size is appropriate for different procedures. We’ll discuss gauge numbers, needle lengths, types of syringes and their compatibility with specific applications.
Understanding Gauge Numbers And Lengths
When selecting the appropriate hypodermic needle for a specific medical application, it is essential to understand the gauge significance and how it relates to both the diameter of the needle and its intended use.
The term ‘gauge’ denotes the thickness or size of a needle, with lower numbers corresponding to larger diameters while higher numbers indicate smaller diameters. Needle materials also play an important role in determining their strength, flexibility, and compatibility with different types of medications.
The length of a hypodermic needle is another crucial aspect that must be considered when choosing the correct size for administration purposes. It is typically measured from the hub (the end connected to the syringe) to the tip (the sharp point).
Longer needles are utilized for deeper injections into muscle tissue or accessing veins, whereas shorter needles are more suitable for subcutaneous injections just beneath the skin’s surface.
Understanding these distinctions between gauge numbers and lengths can significantly impact patient comfort and treatment efficacy during various medical procedures.
| Needle Gauge | Needle Length | Applications |
| 18 | 1 Inch | Moving intramuscular hormones between vial and syringe |
| 21 | 1 or 1 ½ inch | Intramuscular injections such as naloxone, steroids, and hormones |
| 22 | ½ inch | Hormonal intramuscular injections |
| 23 | 1 Inch | Intramuscular injections like naloxone, steroids, hormones, and methadone administration |
| 25 | 1 Inch | Intravenous drug administration, hormone injections, and IV crushed pill delivery |
| 27 | ½ inch | Standard insulin set usage and intravenous drug administration |
| 28 | ½ inch | Intravenous drug use and standard insulin set application |
| 29 | ½ inch | Administering intravenous drugs |
| 30 | ½ or 5/16 inch | Intravenous drug administration |
| 31 | 5/16 inch | Usage for intravenous drug delivery |
Types Of Syringes And Their Applications
Syringes are an essential component in the medical field, as they serve various purposes such as administering medications, drawing blood samples, and providing fluid therapy. The selection of a suitable syringe is vital for performing these tasks effectively and safely.
Numerous factors influence this choice, including the type of procedure being performed, patient’s age and size, medication dosage requirements, and clinician preferences. Syringe materials also play a significant role in determining their suitability for specific applications. Commonly used materials include plastic (polypropylene or polycarbonate) for disposable syringes and glass (borosilicate) for reusable ones.
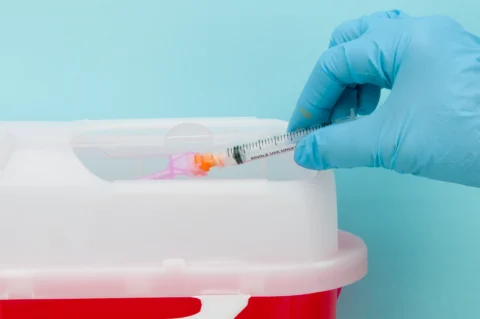
Aside from choosing the appropriate syringe material, it is crucial to consider proper disposal methods after use to prevent cross-contamination and needlestick injuries among healthcare workers. Used sharps should be placed immediately into designated sharps containers that are puncture-resistant, leak-proof, and appropriately labeled or color-coded following local regulations.
Once full, these containers must be securely sealed before disposal through approved waste management services to ensure environmental safety. Furthermore, clinicians should always adhere to standard precautions when handling needles and other sharp instruments to minimize their risk of exposure to bloodborne pathogens during daily clinical practice.
Selecting The Appropriate Needle For Different Procedures
It’s vital to understand the importance of selecting the appropriate needle for different procedures. This selection process should be based on a comprehensive understanding of various factors that can affect patient comfort and safety while ensuring optimal treatment outcomes.
Needle selection factors involve various procedure-specific considerations such as tissue density, injection depth, and medication viscosity.
To make this decision-making process easier, here is a list of general guidelines to help you choose the right needle:
- Gauge: Select a gauge according to the patient’s age, size, and the type of fluid being administered. Higher gauges are thinner needles which cause less pain but may not suit more viscous fluids.
- Length: Choose an appropriate length depending on the target tissue or muscle and consider individual differences in subcutaneous fat thickness among patients.
- Injection site: Consider anatomical landmarks and avoid areas with increased risk of complications (e.g., nerve bundles or blood vessels).
- Patient demographics: Take into account any special needs related to age (pediatrics versus geriatrics), body habitus, cultural preferences or underlying medical conditions.
- Type of procedure: Evaluate whether you need a hypodermic needle for injections (subcutaneous, intramuscular or intravenous) or other specialized needles designed for specific purposes like biopsy, lumbar puncture or regional anesthesia.
Minimizing Patient Discomfort And Ensuring Accuracy
Minimizing patient discomfort and ensuring accuracy during needle-based procedures are crucial aspects of pain management, especially for individuals with needle phobia. Healthcare professionals must consider the appropriate hypodermic needle size to achieve these objectives.
Smaller needles generally cause less pain; however, they may not be suitable for all applications, such as administering viscous medications or drawing blood samples from patients with challenging venipuncture sites. Hence, it is essential to strike a balance between minimizing discomfort and maintaining procedural efficacy when selecting needle sizes.
To address concerns related to pain management and needle phobia, healthcare providers can employ various strategies alongside choosing the right needle size. These approaches include proper skin preparation, utilization of distraction techniques, providing clear communication about the procedure’s steps, and offering reassurance throughout the process.
Employing local anesthetics or numbing agents in certain instances may mitigate any potential anxiety or distress associated with injections or blood draws. By combining thoughtful consideration of equipment choices with compassionate care practices, medical professionals can ensure that their patients experience minimal discomfort while receiving vital treatments or assessments accurately and effectively.
FAQ: Hypodermic Needle Sizes
Q: How do needle gauge sizes differ and why is it important for various types of injections?
A: Needle gauge sizes refer to the outer diameter of the needle, with lower numbers indicating thicker needle walls and higher numbers representing thinner ones. Different gauge sizes cater to various clinical applications, ensuring appropriate needle thickness for specific types of injections such as intramuscular, intradermal, intravenous, and insulin injections.
Q: What factors should be considered when selecting the correct needle size for a particular type of injection?
A: Factors to consider when choosing the right needle size include the patient’s age, weight, and body composition, the type of medication being administered, the desired injection site, and the clinical application. Selecting the appropriate needle size ensures patient comfort and effective delivery of medications.
Q: How does the needle gauge size affect the administration of intramuscular injections?
A: Intramuscular injections require needles that can penetrate deep into the muscle tissue, such as the deltoid muscle. Thicker gauge needles are typically used for this purpose, as they provide better stability and precision during the injection process.
Q: Are there specific needle sizes recommended for insulin injections?
A: Insulin injections are usually administered subcutaneously, meaning the needle must reach the fatty tissue just beneath the skin without penetrating deeper muscles. Thinner gauge needles are commonly used for insulin injections to minimize discomfort and ensure accurate delivery of the medication.
Q: What is the typical range of sizes for hypodermic needle gauges?
A: Hypodermic needle gauges come in a broad range of sizes, usually between 14-gauge (thickest) and 30-gauge (thinnest). The specific gauge needed depends on the type of injection and the patient’s individual needs.
Q: Who were Charles Hunter and Charles Gabriel Pravaz, and how did they contribute to the development of hypodermic needles?
A: Charles Hunter and Charles Gabriel Pravaz were pioneering physicians in the 19th century who independently developed and popularized the use of hollow needles for injecting medications directly into the body. Their work laid the foundation for modern hypodermic needle technology.
Conclusion
It’s crucial for healthcare professionals to understand the various hypodermic needle sizes and their applications. This knowledge ensures that we select the appropriate needles for different procedures, minimizing patient discomfort and maximizing accuracy.
Doing so allows us to provide optimal care for our patients, maintaining both their safety and comfort during injections or other invasive procedures.
Discover the revolutionary Hydra needles at Face Med Shop and elevate your skincare game for a rejuvenated, radiant appearance. Don’t miss out on the chance to experience unparalleled results – visit Face Med Shop today and unlock the secret to youthful, healthy skin!