Regenerative medicine uses Platelet-Rich Plasma (PRP) from a patient’s blood or lab-derived exosomes, tiny messengers containing growth factors, to repair and rejuvenate tissues, but exosomes offer potentially more consistent results than PRP, which varies with age and health.
Understanding the Basics: What is Regenerative Medicine?

Regenerative medicine is a dynamic field focused on repairing, replacing, or regenerating human cells, tissues, or organs to restore normal function. Instead of just managing symptoms, its goal is to address the root causes of disease, injury, and aging. This can involve various approaches, including cell-based therapies (like stem cells), acellular products (like exosomes), and the use of your body’s own healing substances (like PRP).
Platelet-Rich Plasma (PRP) Therapy Explained
What is PRP? The Science Behind Your Body’s Healing Power
Platelet-Rich Plasma, or PRP, is an autologous concentration of platelets in a small volume of plasma, meaning it’s derived from your own blood. Platelets are well-known for their role in blood clotting, but they are also rich reservoirs of growth factors and other bioactive proteins crucial for tissue repair and healing.
Key growth factors found in PRP include Platelet-Derived Growth Factor (PDGF), Transforming Growth Factor-beta (TGF-β), and Vascular Endothelial Growth Factor (VEGF), among others. These substances play vital roles in cell growth, differentiation, and new blood vessel formation, all essential processes for regeneration.
How Does PRP Work? The Mechanism of Action
The mechanism of PRP therapy hinges on harnessing and concentrating these natural healing components. Once PRP is prepared and injected into the targeted area, the activated platelets release a potent cocktail of growth factors.
These growth factors then signal local cells, such as fibroblasts and endothelial cells, to kickstart the healing cascade. This process can stimulate tissue repair, reduce inflammation, promote the formation of new collagen, and improve blood supply to the injured or treated area.
The PRP Procedure: What to Expect
The PRP procedure is typically straightforward and performed in an outpatient setting:
- Consultation: Your clinician will assess your condition and determine if PRP is appropriate for you.
- Blood Draw: A small sample of your blood is drawn, similar to a routine blood test.
- Centrifugation: The blood sample is placed in a centrifuge, a machine that spins at high speed to separate the platelets and plasma from other blood components.
- Preparation: The concentrated platelet-rich plasma is then carefully extracted.
- Injection: The PRP is precisely injected into the targeted area (e.g., an arthritic joint, the scalp for hair loss, or the skin for rejuvenation).
The entire process usually takes about 30 to 60 minutes. Discomfort is generally minimal, though a local anesthetic may be used at the injection site. You can typically resume normal activities shortly after the procedure, with specific post-procedure instructions provided by your clinician.
Common Applications of PRP Therapy
PRP therapy has gained popularity across various medical and aesthetic fields due to its versatility and reliance on the body’s natural healing processes. Common applications include:
- Orthopedics: Treating conditions like osteoarthritis (especially of the knee), tendon injuries (e.g., tennis elbow, Achilles tendinopathy), and ligament sprains.
- Hair Restoration: Stimulating hair growth in individuals with androgenetic alopecia (pattern baldness).
- Skin Rejuvenation: Improving skin texture, tone, and elasticity, reducing fine lines and wrinkles (sometimes referred to as a “vampire facial” when combined with microneedling).
- Wound Healing: Accelerating the healing of chronic wounds, such as diabetic ulcers or surgical incisions.
Benefits and Potential Downsides of PRP
Benefits:
- Autologous: Since PRP is derived from your own blood, there is a very low risk of allergic reactions, immune responses, or disease transmission.
- Minimally Invasive: The procedure involves only a blood draw and injections.
- Promotes Natural Healing: PRP works by stimulating your body’s inherent repair mechanisms.
Downsides/Considerations:
- Variable Results: The effectiveness of PRP can vary depending on the individual’s age, overall health, platelet quality, and the specific condition being treated. This variability is a key consideration, as the concentration and quality of growth factors in your platelets can decline with age or certain health conditions.
- Multiple Sessions Often Needed: Optimal results usually require a series of treatments, typically 2-3 sessions or more, spaced several weeks apart.
- Not a Cure-All: While beneficial for many, PRP is not a guaranteed solution for all conditions.
- Temporary Soreness/Bruising: Mild pain, swelling, or bruising at the injection site is common but typically resolves within a few days.
Exosome Therapy: The Next Frontier in Cellular Communication

What Are Exosomes? Tiny Messengers with a Powerful Impact
Exosomes are nano-sized extracellular vesicles (EVs) – essentially tiny sacs – that are naturally secreted by almost all cell types in the body. They are not cells themselves, but rather complex packages containing a diverse cargo of proteins, lipids, and nucleic acids, including messenger RNA (mRNA) and microRNA (miRNA).
Think of exosomes as tiny delivery trucks, constantly shuttling important molecular information between cells. This intercellular communication is vital for regulating a wide range of biological processes, from immune responses to tissue regeneration.
Where Do Exosomes Come From? Source Matters
The exosomes used in therapeutic applications are commonly derived from mesenchymal stem cells (MSCs). MSCs are multipotent cells that can be obtained from various sources, including ethically donated umbilical cord tissue, bone marrow, or adipose (fat) tissue.
The source and quality of the parent MSCs, as well as the conditions under which they are cultured and the methods used to isolate and purify the exosomes, are critical factors that can significantly influence the composition and therapeutic potential of the final exosome product.
Strict donor screening and quality control measures are paramount for allogeneic (donor-derived) exosome products. While less common in the current therapeutic landscape, research is also exploring plant-derived exosomes and exosomes from other cell types.
How Does Exosome Therapy Work? Delivering Regenerative Signals
Exosome therapy leverages the natural signaling capabilities of these vesicles. When administered, exosomes interact with target cells by fusing with their membranes or being taken up by them. Once inside, they release their bioactive cargo, which can then modulate the recipient cell’s behavior.
For instance, exosome-delivered molecules can instruct cells to reduce inflammation, proliferate (divide and grow), form new blood vessels (angiogenesis), produce more collagen, or protect themselves from damage. The specific effects depend on the molecular contents of the exosomes, which are influenced by their cell of origin.
The Exosome Therapy Procedure: What’s Involved?
Exosome therapy typically involves the administration of a purified exosome product that has been prepared in a laboratory.
- Product Sourcing: Clinicians will use exosome products obtained from reputable specialized labs that adhere to stringent manufacturing and quality control standards. Unlike PRP, a blood draw from the patient is generally not required for allogeneic (donor-derived) exosome products.
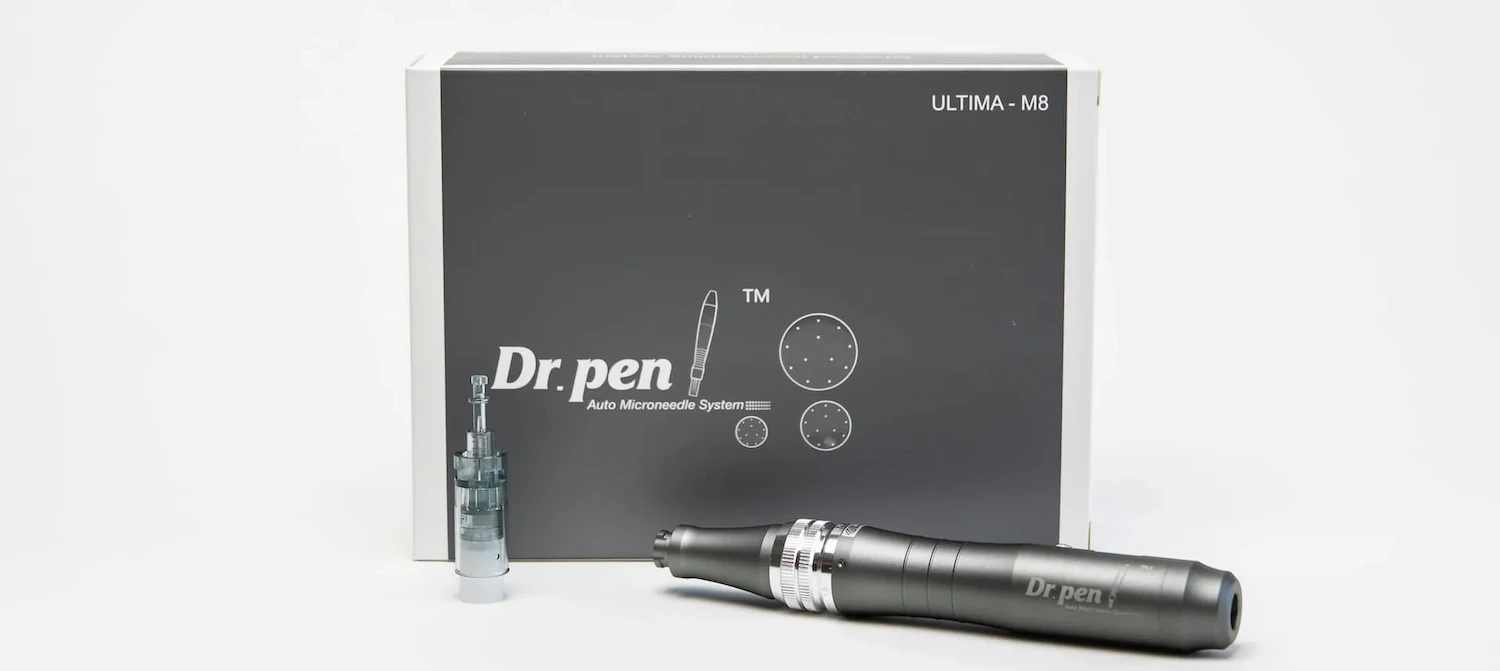
- Administration: Exosomes are most commonly administered via direct injection into the targeted tissue (e.g., a joint, the scalp, or skin) or, in some cases, through intravenous (IV) infusion or topical application, particularly after procedures like microneedling that create channels for absorption.
- Session & Recovery: A typical session is relatively quick. Recovery is usually minimal, with patients often experiencing little to no downtime. Some mild redness or swelling at the injection site may occur but typically subsides quickly.
Common Applications of Exosome Therapy
Exosome therapy is an area of intense research and growing clinical interest, with applications being explored across numerous fields:
- Skin Rejuvenation and Anti-aging: Improving skin texture, elasticity, reducing wrinkles, and promoting a more youthful appearance by stimulating collagen and elastin production and reducing inflammation.
- Hair Restoration: Stimulating hair follicles and promoting hair growth, often cited for potentially potent effects.
- Inflammatory Conditions: Modulating inflammatory responses in conditions like osteoarthritis or other chronic inflammatory diseases.
- Wound Healing: Enhancing tissue repair and regeneration in acute and chronic wounds.
- Emerging Research: Investigational uses in orthopedics (e.g., cartilage repair), neurodegenerative conditions, and other areas are actively being studied.
Benefits and Potential Considerations for Exosome Therapy
Benefits:
- Acellular: Exosomes are not cells, which means there’s no risk of cell rejection or uncontrolled cell growth if sourced and purified properly. This makes them an attractive option, especially with allogeneic products.
- Potent Signaling: Exosomes can carry a high concentration and diverse array of growth factors, cytokines, and regulatory RNAs, potentially offering more potent and multifaceted signaling compared to the growth factors in PRP alone.
- Potential for Consistent Product Quality: When derived from well-characterized MSCs (e.g., from young, healthy donors) and manufactured under controlled conditions, exosome products may offer a more consistent regenerative potential compared to autologous PRP, which can vary based on the patient’s age and health.
- Versatile Applications: Their ability to modulate various cellular processes makes them suitable for a wide range of potential therapeutic uses.
- Low Immunogenicity: Pure exosome preparations typically have low immunogenicity, meaning they are less likely to provoke an adverse immune response.
Considerations:
- Cost: Exosome therapy is generally more expensive per session than PRP, reflecting the complex manufacturing and purification processes involved.
- Regulatory Status: This is a crucial point. Currently, most exosome products for therapeutic use are considered investigational and are not FDA-approved drugs for specific treatments (this will be detailed in a later section).
- Importance of Product Quality/Sourcing: The efficacy and safety of exosome therapy heavily depend on the quality of the source cells, the manufacturing process, and the purity of the final exosome product. Not all exosome products are created equal, and standardization is an ongoing area of development in the field.
- Potential for Mild Side Effects: As with any injection, there can be temporary mild redness, swelling, or bruising at the administration site.
Stem Cell Therapy: Harnessing the Power of Master Cells

Stem cell therapy stands as a pillar in the field of regenerative medicine, centered on the unique capabilities of stem cells-the body’s fundamental building blocks.
These are undifferentiated cells with the remarkable capacity to develop into many different specialized cell types and to self-renew, producing more stem cells . This inherent ability to build, repair, and recover tissue makes them a focal point of intense research and therapeutic development .
What Are Stem Cells? The Foundation of Regeneration
Stem cells are immature cells characterized by two key properties:
- Self-Renewal: They can divide and replicate themselves many times over, maintaining a pool of undifferentiated cells .
- Differentiation: Under the right conditions, they can transform (differentiate) into specialized cells that make up the body’s tissues and organs, such as muscle cells, brain cells, cartilage cells, or blood cells .
This dual capacity allows stem cells to play crucial roles in growth, development, and the ongoing repair of damaged tissues throughout life .
How Does Stem Cell Therapy Work? Direct Regeneration and Repair
Stem cell therapy aims to leverage these natural properties to treat diseases or repair injuries. The mechanisms through which stem cells can promote tissue regeneration are diverse and complex :
- Differentiation and Cell Replacement: Transplanted stem cells can potentially differentiate into the specific cell types needed to replace those damaged or lost due to disease or injury . For example, they might regenerate cartilage in an arthritic joint or repair heart tissue after a heart attack .
- Paracrine Signaling (Release of Bioactive Molecules): Stem cells release a variety of growth factors, cytokines, and other signaling molecules that can influence the behavior of nearby cells. This is similar to how exosomes function, as exosomes are part of this paracrine effect. These signals can:
- Inhibit Inflammation: Modulate inflammatory cascades, which is beneficial in many degenerative and autoimmune conditions .
- Reduce Apoptosis (Programmed Cell Death): Protect existing cells from dying .
- Stimulate Angiogenesis: Promote the formation of new blood vessels, improving blood supply to damaged areas .
- Recruit Local Cells: Attract the body’s own reparative cells to the site of injury .
- Immunomodulation: Certain types of stem cells, particularly Mesenchymal Stem Cells (MSCs), have demonstrated powerful immunomodulatory properties, meaning they can help regulate the immune system. This is valuable for treating autoimmune diseases and preventing transplant rejection .
Sources and Types of Stem Cells Used in Therapy
Various types of stem cells are utilized or investigated for therapeutic purposes, sourced either from the patient themselves (autologous) or from a screened donor (allogeneic) . Common sources include:
- Mesenchymal Stem Cells (MSCs): These are multipotent adult stem cells that can differentiate into bone, cartilage, muscle, and fat cells. MSCs are often obtained from:
- Bone marrow
- Adipose (fat) tissue
- Umbilical cord tissue MSCs are particularly known for their anti-inflammatory and immunomodulatory effects, as well as their ability to support tissue repair .
- Hematopoietic Stem Cells (HSCs): These are blood-forming stem cells typically found in bone marrow. HSC transplantation (e.g., bone marrow transplant) is an established treatment for certain blood cancers and genetic blood disorders .
- Induced Pluripotent Stem Cells (iPSCs): These are adult cells that have been reprogrammed in a lab to an embryonic stem cell-like state. iPSCs hold significant promise for personalized medicine and disease modeling, though their clinical application is still evolving .
The patient’s own condition and prior treatments (like chemotherapy) can impact the quantity and quality of available autologous stem cells. Allogeneic stem cells from healthy, screened donors can sometimes overcome these limitations .
The Stem Cell Therapy Procedure: What’s Involved?
The procedure for stem cell therapy varies depending on the type of stem cells, the source, and the condition being treated, but generally involves:
- Consultation and Evaluation: A thorough medical assessment to determine if stem cell therapy is appropriate.
- Stem Cell Sourcing:
- Autologous: If the patient’s own cells are used, this involves a harvesting procedure (e.g., bone marrow aspiration or fat Lipoaspiration).
- Allogeneic: If donor cells are used, these are typically sourced from a cell bank that processes and stores cells from ethically screened donors.
- Processing and Preparation: Harvested or sourced cells are often processed in a laboratory to isolate and concentrate the stem cells. This may also involve culturing the cells to obtain a sufficient number for therapy, a step that has regulatory implications . Characterizing the identity and purity of the cells before administration is crucial .
- Administration: Stem cells are then delivered to the patient, commonly through:
- Direct injection into the affected area (e.g., an arthritic joint) .
- Intravenous (IV) infusion.
- As part of a tissue-engineered graft .
The quantity of cells required can be substantial, and careful management of the cells is vital throughout the process .
Common Applications of Stem Cell Therapy
Stem cell therapy is being applied or investigated across a wide spectrum of medical conditions :
- Orthopedics: Treating conditions like knee osteoarthritis (KOA) by potentially regenerating cartilage and reducing inflammation .
- Autoimmune Diseases: Modulating the immune response in conditions like multiple sclerosis and rheumatoid arthritis .
- Inflammatory Conditions: Leveraging anti-inflammatory properties for various disorders .
- Neurological Disorders: Investigational treatments for conditions like Parkinson’s disease and spinal cord injuries .
- Cardiovascular Diseases: Repairing damaged heart tissue after a heart attack .
- Blood Cancers and Disorders: Established use of HSC transplantation (bone marrow transplant) for leukemia, lymphoma, and other conditions .
- Wound Healing and Tissue Repair: Regenerating skin and other tissues.
Success rates can vary, with recent research indicating ranges from 50% to 90% in different regenerative applications, and specific positive outcomes noted in areas like joint repair and autoimmune conditions (around 80%) .
Benefits and Potential Risks/Considerations of Stem Cell Therapy
Benefits:
- Regenerative Potential: Offers the possibility of repairing or replacing damaged tissue, rather than just managing symptoms .
- Broad Applications: Shows promise across diverse medical fields .
- Immunomodulatory Effects: MSCs, in particular, can help regulate the immune system and reduce inflammation .
- Personalized Medicine Potential: Especially with autologous cells or iPSCs, treatments can be tailored .
- Curative Potential in Some Cases: HSC transplantation is a curative therapy for certain blood cancers .
Risks and Considerations:
- Cell Viability and Engraftment: A significant concern is ensuring that transplanted stem cells survive, integrate into the target tissue, proliferate appropriately, and effectively regenerate tissue
- In Vitro Manipulation: Genetic and epigenetic changes can occur when cells are manipulated or expanded in culture outside the body, potentially impacting their safety and efficacy .
- Immune Rejection: While less common with MSCs (which are somewhat immune-privileged) or autologous cells, allogeneic stem cells can still pose a risk of immune rejection, potentially requiring immunosuppressive drugs .
- Tumorigenicity (Risk of Cancer): There’s a theoretical concern that transplanted stem cells, especially pluripotent ones or those not properly differentiated, could form tumors due to their replicative capacity. Thorough characterization of the cells before administration is critical to mitigate this risk .
- Side Effects: As with any injection, localized pain, swelling, or effusion (fluid buildup) can occur, as reported in some KOA studies . Other common adverse reactions may also be possible.
- Quality and Source of Cells: The quality, purity, and characterization of the stem cell product are paramount for safety and efficacy .
- Regulatory Status: Many stem cell therapies are still investigational and not yet FDA-approved for widespread clinical use outside of strictly regulated clinical trials or specific established treatments (like HSC transplantation for certain conditions). Patients should be cautious of unproven treatments and ensure any therapy is provided under appropriate regulatory oversight. The FDA has issued warnings about unapproved stem cell products.
- Cost: Stem cell therapies can be expensive, reflecting the complex procedures involved in harvesting, processing, and administering the cells.
Mechanism of Action: How Do They Trigger Healing?

PRP: Works primarily by releasing a localized burst of growth factors from the activated platelets at the site of injury or treatment. These growth factors then act as signals to stimulate the body’s natural healing processes, like cell proliferation and new tissue formation.
Exosomes: Function as more sophisticated intercellular messengers. They deliver their diverse cargo of biomolecules directly into target cells, influencing a wider range of cellular functions.
This can include not only stimulating repair and regeneration but also powerfully modulating inflammation, promoting angiogenesis (new blood vessel formation), and even transferring genetic information (like miRNAs) that can alter cell behavior in a more nuanced way.
Stem Cells: Operate through multiple mechanisms. They can directly differentiate into specialized cells to replace damaged or lost tissue. Additionally, and often more significantly, stem cells (particularly Mesenchymal Stem Cells or MSCs) exert powerful paracrine effects by releasing a broad array of growth factors, cytokines, and extracellular vesicles (including exosomes).
The Impact of Source and Quality: Why It Matters (UVP Focus)
PRP: A critical factor influencing PRP’s effectiveness is the patient’s own biological status. As individuals age, or if they have certain underlying health conditions or systemic inflammation, the number and quality of their platelets, and consequently the concentration of beneficial growth factors in their PRP, can diminish.
This means that PRP prepared from an older individual or someone with health issues might be less potent than PRP from a young, healthy person. Medications like NSAIDs can also impact platelet function.
Exosomes: High-quality exosome products, particularly those derived from young, healthy donor MSCs (like those from umbilical cord tissue) and manufactured under standardized, controlled conditions, aim to provide a more consistent and potentially more potent regenerative signal.
Because they are sourced from carefully selected and cultured cells, their molecular profile can be more reliably characterized and less dependent on the recipient patient’s age or health status. This consistency is a key theoretical advantage. However, it’s crucial to emphasize that not all exosome products are created equal; purification, characterization, and quality control are paramount.
Stem Cells: The source, type, and condition of stem cells are paramount for therapeutic outcomes. For autologous (patient-derived) stem cells, factors like the patient’s age, underlying diseases, and prior treatments (e.g., chemotherapy) can significantly affect the quantity and regenerative capacity of the harvested cells. Allogeneic stem cells from healthy, screened donors (e.g., MSCs from umbilical cord tissue) can offer more robust and consistent cell populations.
However, the “initial conditions,” including the graft source and any in vitro manipulation (culturing, expansion), can influence cell behavior, epigenetic states, and differentiation potential, which in turn impact their therapeutic efficacy and safety. Rigorous processing, characterization for identity and purity, and quality control are vital for any stem cell therapy to ensure viability and minimize risks like genetic changes or unwanted differentiation.
Efficacy and Consistency: What Do Studies Suggest?
- PRP: There is a considerable body of research on PRP for various conditions, particularly in orthopedics (like knee osteoarthritis) and for hair restoration, with many studies showing positive outcomes. However, results can be inconsistent across studies, partly due to variations in PRP preparation methods, patient populations, and the inherent variability of autologous products.
- Exosomes: Research into exosome therapy is rapidly expanding and shows significant promise across a range of preclinical and early-phase clinical studies for conditions including skin aging, hair loss, wound healing, and inflammatory joint diseases. Exosomes are often reported to have potent anti-inflammatory and regenerative effects. However, as a newer therapeutic modality, more large-scale, long-term, and comparative human clinical trials are needed to fully establish efficacy, optimal dosing, and long-term safety for many specific clinical indications.
- Stem Cells: The efficacy and consistency of stem cell therapy can vary significantly based on the type of stem cells used, the condition being treated, the delivery method, and patient-specific factors. Mesenchymal Stem Cells (MSCs) have shown promise in preclinical models and clinical trials for a range of conditions including stroke, liver cirrhosis, premature ovarian failure, and ARDS, often demonstrating anti-inflammatory and neuroprotective properties. However, while safety is often reported, particularly for MSCs , definitive efficacy in large-scale human trials is still being established for many applications.
FDA Approval & Regulatory Landscape: A Crucial Consideration
Navigating the regulatory status of regenerative therapies like PRP and exosomes can be confusing. It’s vital to understand the current landscape.
PRP: FDA Cleared Devices vs. Approved Uses
It’s important to differentiate between “FDA cleared” and “FDA approved.” The U.S. Food and Drug Administration (FDA) clears medical devices used to prepare PRP, such as centrifuges and specialized collection kits. This clearance means the FDA has determined these devices are substantially equivalent to an already legally marketed device and are safe for their intended use (i.e., preparing PRP from a patient’s blood).
However, this device clearance is not the same as the FDA approving PRP as a “drug” or “biologic” for treating specific diseases or conditions. The actual use of PRP for various medical applications (e.g., injecting it into a knee for arthritis or into the scalp for hair loss) is generally considered the “practice of medicine.”
This means that licensed healthcare providers can use FDA-cleared devices to prepare PRP and administer it for various indications, but these specific uses of PRP itself are not individually FDA-approved as treatments for those conditions.
Understanding FDA terminology can be tricky. While the tools used to prepare PRP are cleared by the FDA, similar to how a syringe is cleared, the specific use of PRP for treating, say, knee arthritis, isn’t individually approved as a ‘drug.’
Exosomes: The Regulatory Path for Acellular Products
Exosome products intended for therapeutic use (i.e., to treat, prevent, or cure a disease or condition) are generally regulated by the FDA as drugs or biologics. This regulatory pathway is much more rigorous than that for medical devices.
For an exosome product to be legally marketed in the U.S. for a specific therapeutic indication, it typically requires an Investigational New Drug (IND) application to be filed with the FDA, followed by extensive clinical trials (Phase I, II, and III) to demonstrate both safety and efficacy for that specific use. Only after successful completion of these trials can a manufacturer seek FDA approval.
Currently, there are no FDA-approved exosome products for the treatment of any specific disease or condition for widespread clinical use outside of regulated clinical trials. Some clinics may offer exosome therapies under specific research protocols (e.g., IRB-approved studies) or for compassionate use in certain situations, but patients should be wary of any claims that exosome products are “FDA approved” for general therapeutic applications if this is not accurate. The FDA has issued consumer warnings about unapproved stem cell and exosome products.
Stem Cells: Navigating FDA Regulations for Cellular Therapies
Stem cell therapies, being cellular products, also fall under stringent FDA regulation, typically as drugs or biologics, especially when more than minimally manipulated or intended for non-homologous use (i.e., performing a different basic function than in the donor).
The FDA’s Center for Biologics Evaluation and Research (CBER) oversees these products, often classifying them as “section 351 products,” which require premarket approval, including an Investigational New Drug (IND) application and robust clinical trial data demonstrating safety and efficacy .
This means that for most stem cell therapies aimed at treating specific diseases:
- An IND application must be submitted to and cleared by the FDA before clinical trials can begin.
- Extensive clinical trials (Phase I, II, and III) are necessary to establish safety and effectiveness.
- Only after successful completion of these trials can a Biologics License Application (BLA) be submitted for FDA approval.
There are some established and FDA-approved stem cell therapies, primarily hematopoietic stem cell (HSC) transplantations (e.g., bone marrow transplants) for certain cancers and blood disorders. More recently, the FDA has approved some specific mesenchymal stem cell (MSC) therapies, such as Ryoncil (remestemcel-L), for steroid-refractory acute graft-versus-host disease (aGvHD) in pediatric patients, marking a significant milestone for MSC-based therapies .
However, for many other advertised stem cell treatments, particularly those offered directly to consumers for a wide range of conditions outside of FDA-approved protocols, they are considered investigational and unapproved.
The FDA has issued numerous warnings about clinics marketing unapproved and potentially harmful stem cell therapies. Patients should exercise extreme caution and verify the regulatory status of any stem cell treatment offered, ensuring it is part of an FDA-approved clinical trial or is an FDA-approved product for their specific condition.
Why Regulatory Status Matters for Patients

The regulatory status of a medical product has significant implications for patients:
- Safety and Efficacy: FDA approval (for drugs/biologics) or clearance (for devices) provides a level of assurance that the product has been reviewed for safety and, in the case of approval, proven efficacy for its intended use through rigorous scientific evaluation.
- Marketing Claims: Products that are FDA-approved can be legally marketed for their specific approved indications. Unapproved products may sometimes be marketed with claims that are not substantiated by robust clinical evidence.
- Quality Control: FDA oversight helps ensure that manufacturing processes meet certain quality standards. It’s crucial for patients to have open discussions with their healthcare providers about the regulatory status of any proposed treatment, the evidence supporting its use for their specific condition, and any potential risks involved.
Making the Choice: Which Therapy is Right for You?
Deciding between PRP and exosome therapy, or any medical treatment, is a personal journey that should always be undertaken in close consultation with a qualified healthcare professional. This guide aims to arm you with information, but your doctor’s expertise is paramount in tailoring a treatment plan to your unique circumstances.
Factors to Consider with Your Doctor
When discussing your options, here are key factors to consider:
- Your Specific Condition and Its Severity: Is it a mild, acute issue, or a more chronic, advanced condition? Some therapies may be better suited for certain stages or types of problems.
- Your Age and Overall Health: As discussed, these factors can significantly influence the potential quality and efficacy of your own PRP. If your healing capacity might be compromised, exosomes could be a consideration.
- Treatment Goals and Expectations: What are you realistically hoping to achieve? Are you looking for symptom relief, functional improvement, aesthetic enhancement, or true tissue regeneration?
- Scientific Evidence for the Specific Application: Discuss the available research supporting the use of PRP or exosomes for your particular condition. How strong is the evidence?
- Cost and Budget: Consider the per-session cost and the likely number of sessions needed for each therapy, and how that fits into your budget.
- Provider Experience and Qualifications: Ensure your provider is experienced in administering these therapies and can explain the rationale for their recommendations.
- Your Comfort Level with Autologous vs. Allogeneic Products: Some individuals have a strong preference for using only their body’s own materials (autologous, like PRP), while others may be open to well-screened, lab-derived allogeneic products (like many exosome therapies).
Finding a Qualified Provider for PRP or Exosome Therapy

Choosing the right clinician is as important as choosing the right therapy.
- Research Clinics and Practitioners: Look for providers with specific training and substantial experience in regenerative medicine and the particular therapy you are considering. Check credentials, read patient reviews, and assess their reputation.
- Questions to Ask During a Consultation:
- What is your experience with [PRP/Exosome] therapy for my specific condition?
- What are the potential benefits and risks in my case?
- What is the source of the exosomes you use, and what quality control measures are in place (for exosome therapy)?
- How is the PRP prepared in your clinic (for PRP therapy)?
- What results can I realistically expect, and over what timeframe?
- How many sessions do you anticipate I will need?
- What is the full cost of the treatment course?
- What is the regulatory status of the treatment you are proposing for my condition?
- Importance of Transparency and Realistic Expectations: A qualified provider will offer a balanced perspective, discuss potential limitations as well as benefits, and avoid overpromising results. They should be transparent about costs and procedures.